Patient Education Resource Center
As a national leading provider of senior healthcare services, Consulate Health Care is pleased to provide patient education resources for the health conditions that are most prevalent among our elderly population. Below, you will find the topics for each of the nine educational resources. By clicking on any of these topics, you will be able to access information about the medical condition, symptoms, treatment and much more. We hope you find these resources helpful and will consider the compassionate and caring services of Consulate Health Care for all of your senior healthcare needs.
If you found an error, highlight it and press Shift + Enter or click here to inform us.
Multiple Sclerosis
Multiple Sclerosis (MS) is a disease of the central nervous system. With MS, damage and deterioration happens to the myelin sheath.
The Central Nervous System (CNS) is made of the brain, spinal cord and nerves. Nerve cells carry electrical impulses from the brain to all of the muscles and organs of the body. This impulse makes the muscles move and the organs function as they should.
The Myelin Sheath is a fatty substance that acts as a protective coating surrounding all nerve cells, like the coverings you see on electrical wires. This coating helps to insulate the nerve and help the impulse flow through strongly and quickly. With MS, the damage to the myelin sheath creates interference in the communication that normally occurs between the brain, spinal cord and other areas in the body. The electrical impulse is “scattered” and weakened by the lack of “insulation”. Messages carried along the central nervous system routes slow down or stop.
The damage is not caused from trauma. The cause is not fully understood however, research suggests that MS is an abnormal autoimmune response in people who have specific genetic susceptibility. This means that the person’s own immune system attacks the nerve and the destruction is caused from the inflammation of that “attack”. When people who possess this gene are exposed to environmental factors, such as a virus, the inflammatory response is triggered and activated.
Who seems more at risk to develop MS?
- Onset generally occurs between the age of 20-40 years
- Women are two times more likely to develop MS than men
- Men tend to have later onset and potentially worse prognosis
- Family history increases risk (20-30 times more common to first relatives)
- Certain infections and a variety of viruses increase risk
- Individuals with roots originating in northern Europe
- Geographic regions: southern Canada, northern USA, New Zealand, SE Australia (scientists have identified an “MS Belt”)
Symptoms of Multiple Sclerosis
Symptoms depend on the amount of damage and the types of nerves effected with each attack. The disease is unpredictable, and symptoms can range from relatively benign or mild, to devastatingly disabling. The condition is characterized by cycles of periods of disease freedom, or remission to relapses or new attacks with multisystem dysfunction. With each new attack, symptoms may change.
MS is chronic and incurable. It is a progressive, irreversible and debilitating condition. MS is not a “terminal” condition. This means that people with MS do not die from MS attacks, but may develop terminal “complications” of MS such as:

Respiratory disease is the most common cause

Heart Disease is common and difficult to control as physical activity is limited

Higher risk for
infections related
to medication side
effects and bladder
dysfunction

Risk of aspiration (choking) related to swallowing problems

Muscle symptoms can be mild or totally debilitating
- Loss of balance and trouble walking
- Muscle spasms and weakness
- Coordination of limbs involving fine or gross motor skills
- Tremors in one or more arms and legs
- Seizures

Bowel and bladder symptoms
- Urine incontinence
- Urinary frequency or urgency
- Difficulty beginning urine stream
- Constipation
- Bowel incontinence

Eye symptoms
- Eye pain
- Uncontrollable eye movements
- Double vision
- Lost vision, commonly in one eye

Sensory changes
- Painful spasms
- Facial pain
- Tingling, crawling or burning sensation to limbs
- Hearing loss
- Dizziness and excessive fatigue

Cognitive changes
- Decreased attention span
- Memory loss
- Poor judgment
- Difficulty reasoning
- Difficulty problem solving
- Depression

Speech & swallowing symptoms
- Slurred or speech that is difficult to understand
- Problems chewing
- Swallowing difficulties with aspiration risk

Sexual changes
- Erectile dysfunction
- Poor vaginal lubrication
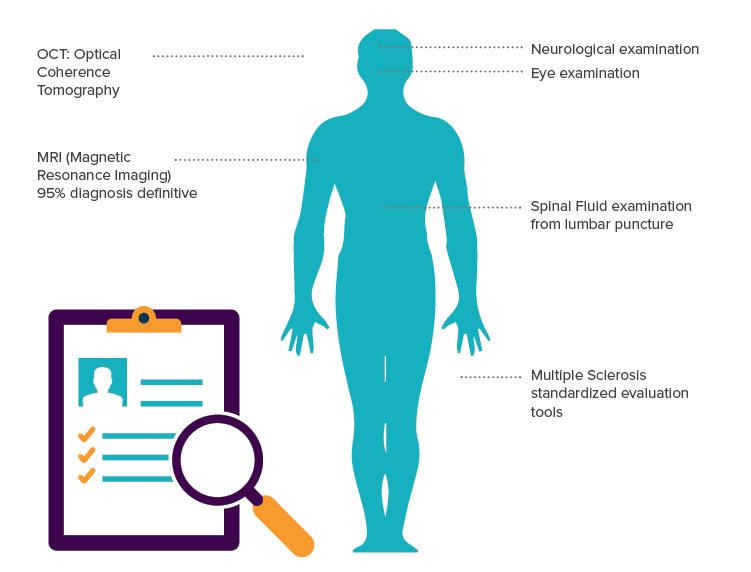
The Diagnosis Process
The diagnosis of MS sometimes requires comparisons of test results and symptoms. Some tests that may be used are:
Disease Management Goals
- Decreasing the frequency and number of relapses
- Limiting disability and optimizing functionality
- Symptom managment
- Supportive ADL assistance
- Support acceptance of changes in body as it relates to appearance and performance
Medication Therapy and MS
Some medications that are used are listed below. All medications have side effects; many MS medications can have severe side effects. Also, some medications work better for some, and not as well for others. The treatment plan regarding medications must be discussed with your primary care provider so that together you can decide what the risks and benefits are:
Medications to Modify or Slow the Disease Process
- Beta Interferons Injections: Avonex, Betaseron, Extavia, Rebif. These drugs attempt to slow the MS progression, and reduce the frequency and the severity of attacks. Routine blood tests must be performed to monitor blood count and liver function. Side effects include: flu-like symptoms and depression.
- Glatiramer acetate injection: Copaxone. This drug works by attempting to lock the immune system’s attack on the myelin sheaths of the nerve cell. It may cause flushing, rapid heart rate with chest pain and local reactions noticed at the injection site.
- Teriflunomide: Augagio. This medication reduces swelling and inflammation in the nervous system. Tests must be performed to monitor liver function and blood pressure. Pregnancy is contraindicated during administration and for two years thereafter.
- Fingolimod: Gilenya. This medication works by trapping immune cells within the lymph nodes, inhibiting them from migrating into the brain and spinal cord. It must be used with effect include heart slowing, heart rhythm blocking, eye swelling, headache, infections, high blood pressure, diarrhea, liver dysfunction and respiratory disorders. One must be immune to chicken pox to receive this medication.
- Natalizumab infusion: Tysabri. This medication interferes with the immune cell movement in the blood stream from the brain and spinal cord. It is reserved only for use in relapsing symptoms of MS with increased frequency and substantial disability. The medication has many serious and potential life threatening side effects and is used with caution.
- Mixoxantrone infusion: Novantrone. This is a potent immunosuppressive medication, reserved only for use in relapsing symptoms of MS with increased frequency and substantial disability. It has been known to be harmful to the heart and associated with cancer development such as leukemia. Generally, it is used only to treat the most severe cases.
Medications to Treat Symptoms
It is not uncommon to receive medications that manage just symptoms. Common difficulties that may receive pharmacologic interventions include:
- Spasticity and body movement
- Bladder dysfunction
- Bowel dysfunction
- Fatigue
- Depression
- Pain
- Seizures
Inflammation At The Cellular Nerve Level
Corticosteroids: Prednisone (Deltasone) orally, Decadron or Solu-Medrol can be administered into muscles or veins. These medications are mainly used to reduce the inflammation during a relapse. They may be prescribed to be administered intravenously using a pump or orally. Side effects include mood swings, weight gain, and increased risk of infection.
Body Movement
Dalfampridine: Ampyra This medication is called a “potassium channel blocker”. It is mainly used to progress walking abilities. It works by trying to improve the transmission of impulses along the nerve pathways. With the damage of myelin sheaths present with MS, potassium ions can easily ooze from nerve fibers, disrupting cellular communication and impulses. By blocking these potassium channels, communication is increased and nerve function may be improved. Side effects include dizziness, headache, nausea, weakness, insomnia and urinary tract infections.
Spasticity
Muscle Relaxants: Baclofen (Lioresal) and Tizanidine (Zanaflex). Many individuals with MS suffer from painful and uncontrollable muscle stiffness and spasms of the legs. These medications are prescribed to reduce muscle spasticity. Side effects include sedation and problems thinking.
Bladder Problems
MS often causes bladder dysfunction that negatively impacts storage, emptying or both. Incontinence is frequently associated with urgency and a spastic bladder. Medications may be prescribed such as Oxybutynin (Ditropan) or Tolterodine (Detrol) may help in early stages
Bowel Issues
Bowel management often involves addressing constipation and incontinence. Often pharmalogical products such as suppositories, bulk forming products, stool softeners, or laxatives.
Fatigue Medicine
Fatigue has been identified as the most common and disabling MS symptom. Fatigue can be caused by the disease itself, or experienced as a result of another medical condition or a medication side effect. Other conditions that can contribute to fatigue with MS include depression, pain, thyroid dysfunction, anemia, low levels of Vitamin B12 and insomnia. Medications that can help with fatigue are drugs that stimulate the central nervous system. The most common medication used is Amantadine (Symmetrel) although this is considered “off label” prescribing for MS fatigue. Other stimulating medications used are Methylphenidate (Ritalin) Modafinil (Provigil) and Pemoline (Cylert). Side effects include restlessness, increased spasticity and sleeplessness.
Medication For Mood Problems
Depression has been linked to brain changes in people with MS. It is also a side effect of beta interferon, a commonly used medication.
Depression is significant in the MS population. Suicide rates are twice that of the non-MS population and suicidal thoughts are even higher. MS can be associated with alcohol abuse and social isolation. Some medications that are commonly used to help with mood are SSRI antidepressants such as Sertaline (Zoloft) and fluoxetine (Prozac) because of their ability to energize and uplift. Tricyclic antidepressants may also be used to enhance willingness to be more active and to stabilize moodiness. These medications are Amitriptyline (Elavil) and Nortriptyline (Pamelor).
Pain
The sensory system is usually responsible for the pain experienced with MS. Complaints of pain are usually burning or pressure feelings to extremities and back. A common symptom that seems to come and go is known as “ Lhermitte sign”. This is a shock like sensation, shooting down the trunk or limbs when the neck is moved and described as “lightening”. MS also causes headaches, facial pain, eye pain and pain associated with spasms of the arms and legs. Over the counter, nonsteroidal anti-inflammatory medications are usually prescribed along with medications addressing other symptoms, like spasms, that are attributing to the pain experience.
Seizure
Research has shown that epileptic seizures are three to six times more likely in people with MS than people who do not have this disease. Seizure activity is controlled by anticonvulsant medications. Additionally, these types of products assist in reducing sensory pain sensations and intermittent spasms occurring from spinal cord irritation. Drugs most commonly prescribed are Carbamazepin ( Tegretol) Gabapentin (Neurotin) and Lamotrigine (Lamictal).
Vitamin Supplementation
Vitamin B supplements are often prescribed to support nerve cell function and enhance a sense of wellbeing and energy. This includes the B-Vitamin complex, but especially Vitamin B12, under the tongue. This vitamin aids in protecting the myelin sheath and cellular longevity.
Non-Medicinal Treatment for MS
There are many things that you can do to help the medications work or to combat symptoms without medications such as:

Pain: Keeping as active as possible, light exercise and range of motion stretching can keep muscles and joints healthier, decreasing the pain sensation.

Constipation: Constipation can be lessened by drinking plenty of fluids through the day as well as assuring that you eat items that have high fiber content, such as your fruits and vegetables, and by staying active.

Depression: If a sad mood occurs, be sure to express your feelings to loved ones, if feelings become overwhelming let staff know so that additional services can be considered. In general, attempt to find and do things that you enjoy, maintain relationships with people for support and stay as active as you can.

Physical & Occupational Therapy Department
(Your Primary Care Provider may order therapy)
The facility physical and occupational therapists can help:
• Design pain management strategies
• Assist with gradual gait and transfer training
• Improve strength and endurance through supervised exercise
• Provide and train with assistive devices and adaptive equipment
• Educate on energy conservation techniques
• Plan and schedule rest to maximize energy

Dietary Staff
The dietician at our facility can meet with you to plan for your preferences. Menu planning will also be aimed at:
• Adequate and fortified nutrition and hydration
• Textures for swallowing successes
• Foods to assist with constipation challenges
• Energy foods for fatigue management
• Adaptive utensils for self-help support

Speech and Language Specialists
(Your Primary Care Provider may order speech therapy)
Effective communication and swallowing may be challenging with MS. It may seem like food gets lodged in your mouth causing coughing or choking or speech seems slurred or distorted. Speech therapy focuses on improving movement of the mouth and facial muscles. Our Speech and Language specialist can meet with you to:
• Provide oral motor exercises and voice training
• Training related to forming language and abstract reasoning
• Processing and problem solving exercises
• Assists in planning, sequencing and prioritizing activities
• Identify and review swallowing sensations and food temperature
• Discuss dietary modifications and food consistencies
• Suggest alternative dining positions for safer and easier swallowing
• Environmental adaptations and caregiver approaches
If you found an error, highlight it and press Shift + Enter or click here to inform us.