Patient Education Resource Center
As a national leading provider of senior healthcare services, Consulate Health Care is pleased to provide patient education resources for the health conditions that are most prevalent among our elderly population. Below, you will find the topics for each of the nine educational resources. By clicking on any of these topics, you will be able to access information about the medical condition, symptoms, treatment and much more. We hope you find these resources helpful and will consider the compassionate and caring services of Consulate Health Care for all of your senior healthcare needs.
If you found an error, highlight it and press Shift + Enter or click here to inform us.

Diabetes Mellitus
Diabetes Mellitus is a chronic disease, requiring lifelong management of food, exercise and medication. There is no cure. The condition is characterized by hyperglycemia-high levels of blood glucose or “high blood sugar”. This is due to not having enough insulin being manufactured by the pancreas. The result is that the body can suffer from disturbances on how carbohydrates, proteins and fat are used.
As food is ingested, the digestive system breaks down sugar and starch (carbohydrates) into glucose, a very simple sugar. This glucose is carried by the blood stream to be used by all the cells of the body. Glucose is essential to health because it is an important source of energy for the all organs and muscles of the body. Glucose is the “food” or “fuel” of the cell. Without it, the cells and organs of your body cannot function.
Insulin is a hormone that transports glucose from the blood- into the cell. Without insulin, glucose cannot get from the blood into the cell to power the cell. Diabetics have too much glucose circling around in their bloodstream and not enough glucose inside the cells where it belongs to create energy.
The result is that the cells of the body, all the organs and tissues and muscles, don’t get the energy they should have. Also, the high levels of glucose circulating in the bloodstream, over time, can cause problems in the body.
What is Insulin?
Insulin is a hormone that is produced by the pancreas and essential to regulate carbohydrates and fat as they are used in the body. Insulin helps your cells to “use” the blood’s glucose as energy, it acts like a transporter that brings the glucose in the cell to be used. Insulin also triggers cells in the liver, skeletal muscles and fat tissue to absorb glucose from the blood, taking it out of circulation. Insulin acts again, as a transporter to bring glucose into the skeletal muscles and liver to store. The muscles store glucose as glycogen and fat cells store glucose as triglycerides.
The Basics On How Insulin Works
- In the absence of diabetes, insulin is primarily manufactured and released by the pancreas to reduce elevated glucose (sugar) levels from the blood and “drive” that Glucose to the cells to be used or stored.
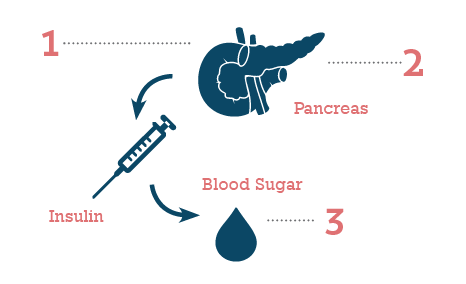
- When sugar levels drop, the pancreas slows or stops the release of Insulin.
- When blood sugar falls below a certain level, the body uses stored glucose as an energy source.
Types of Diabetes
Type 1 Diabetes
The beta cells of the pancreas do not produce insulin because the immune system has attacked and destroyed them. Formerly called “Juvenile Diabetes”.
Type 2 Diabetes
Formally known as “Adult Onset”; 95% Diabetics are Type 2. There are a few ways that it occurs. Sometimes the pancreas does not create enough insulin for the body to use, sometimes the body does not use the insulin effectively, the cells become resistant to the insulin and the “transport” part of insulin does not work well. Sometimes it is a combination of the two problems.
Often associated with:
• Age
• Excess weight
• Physical inactivity
• Hypertension
• Family history
• Abnormal cholesterol and triglyceride levels
• Gestational diabetes
• Polycystic ovary syndrome
• Race: Black, Hispanic, Asian, American Indian
Fast Facts On Diabetes
Diabetes affects 25.8 million people of all ages

8.3 percent of all Americans
Diagnosed: 18.8 million
Undiagnosed est.: 7.0 million
Seventh Leading cause of death in USA
Direct & Indirect costs estimated: $174 billion
Symptoms Of Diabetes
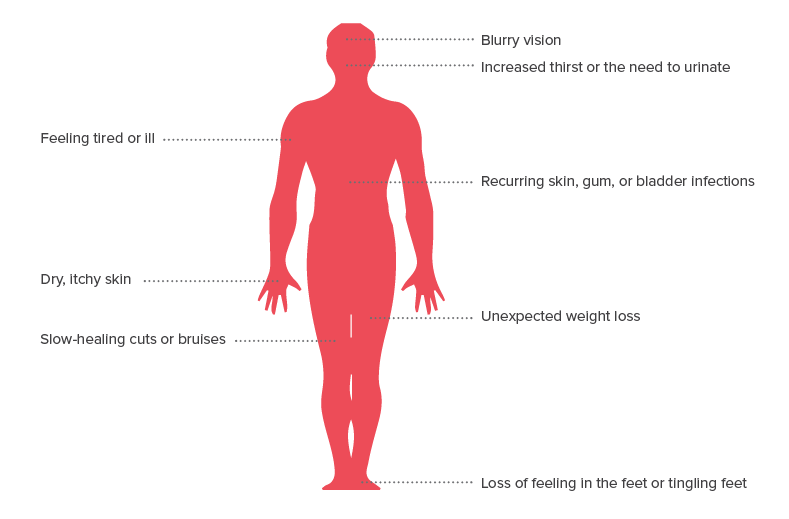
Symptoms of HIGH BLOOD SUGAR:
Even if your diabetes is well controlled, blood sugar may elevate if you have an infection, fever, vomiting, diarrhea, recent surgery, a new illness or change in medications. Please tell the clinical staff if you feel any of the following symptoms associated with high blood sugar:
- Not thinking clearly
- Blurred vision
- Sluggishness, weakness or drowsiness
- Sudden red and dry skin
- Behavior changes
- Frequent Urination/ Incontinence that is new
- Unexplained weight loss in a short time
- Increased thirst
High blood sugars are not always symptomatic, but over time can do damage to the body. High blood sugar levels are treated with insulin.
Diabetic Ketoacidosis is a serious condition that can occur, symptoms include:
- Excessive thirst
- Frequent urination
- Nausea and vomiting
- Abdominal pain
- Weakness or fatigue
- Shortness of breath
- Fruity-scented breath
- Confusion
Symptoms of LOW BLOOD SUGAR:
- Confusion or exhaustion
- Hallucinations
- Irritability/aggressiveness
- Shakiness or tremors
- Blurred vision
- Extreme hunger
- Extreme perspiration
- Dizziness
- Unclear thoughts, unclear speech
- Racing heart
- Numbness or tingling to hands, feet or lips
- Stupor and/or coma
Low blood sugars can create symptoms very quickly and can be dangerous. Treatment usually consists of ingesting or injecting sugar, but may vary according to the situation.
What makes blood glucose levels go too low
- Eating less than usual
- Being more physically active than usual
- Missing a meal or snack
- Eating later than usual
- Diabetic with too much medication
- Drinking alcoholic beverages on an empty stomach
It Is Essential To Call A Nurse If You Feel The Above Symptoms
The long term effects of diabetes and high blood glucose levels can be:
- Increased risk for infection
- Slow healing
- Peripheral Neuropathy- or nerve damage to the hands and feet. This is a condition or disorder of the peripheral nerves — the motor, sensory and autonomic nerves that connect the spinal cord to muscles, skin and internal organs. It usually affects the hands and feet, causing weakness, numbness, tingling and pain. The diabetic with neuropathy often cannot feel the discomfort of sores or pressure to the feet.
- Peripheral Vascular Disease – damage to the blood vessels of the extremities.
- Circulatory and Cardiac Disease
- Kidney Disease
- Serious vision problems including Macular Degeneration- a disorder of the eyes that cause a “blind spot” which gradually worsens over time.
- Periodontal Disease
Understanding The Goals of Treatment with Diabetes
Diet control / weight management
The care center dietician as well as the clinical staff can assist you in diet control and weight management. The following items are learning objectives that should be considered prior to your return home:
- Understanding healthy sources of carbohydrates, protein and fat
- Making healthy food choices
- Adjusting portion sizes
- Reading labels
- Counting carbohydrates
- Planning and preparing meals
- Successful adjustments when dining outside the home
- Adjusting intake to level of activity
Glycemic control
This is a method for blood sugar management.
The Glucometer: is a blood glucose testing machine. It will show how much glucose is in the blood at a given point in time. Your Primary Care Provider will give orders as to when testing should be done. Many people use the results to adjust their insulin doses. Work with the clinical department to practice proper use of the glucometer. Prior to discharge, you can establish times to test your blood sugar and when and who to call if the numbers are too high or too low.
A1C testing: This is a blood test that measures your average blood sugar level over a period of several months and a very good test to measure if your blood sugar management plan is working. The American Diabetes Association recommends this level to be below 7 percent. You should know what your particular A1C target is.
Medication

Oral Medication
Some oral medications stimulate the pancreas to manufacture or release more insulin. Others slow the release of glucose from the liver, requiring less insulin in the body. A combination of medications may be used.

Insulin
When Insulin is prescribed for a diabetic, it is usually because their pancreas cannot produce enough Insulin to meet the body needs. The diabetic takes Insulin to keep blood sugar levels in a safe range by moving glucose from the blood into the cells of the body.
Insulin is available in short, intermediate, long acting and combination preparations. For example; Insulin that is short acting will start to work shortly after taking it. Long acting Insulin may be taken at night to work early the next morning. Insulin is typically injected using a needle and syringe.
Things that you can do to help

Physical Exercise
Exercise can do the following:
- Lowers blood glucose levels
- Lowers blood pressure
- May lower bad cholesterol and raise good cholesterol
- Improve the body’s ability to use insulin
- Keep the heart and bones strong
- Keep the joints flexible
- Lower the risk of falling
- Assist in weight reduction
- Reduce body fat
- Provide more energy
- Reduce stress and elevate mood
Your Primary Care Provider may order physical therapy to help improve strength, balance and endurance.

Foot Care
Diabetics are at high risk for foot ulcerations, especially diabetics with poor blood flow or neuropathy so caring for feet is important.
Common foot issues like calluses, blisters, dry skin and athletes’s foot put the diabetic at risk for infection, which must be met with aggressive care. Toe nails should be trimmed regularly. Podiatric services are available, if ordered. Report any changes in skin condition to the clinical staff promptly. Report redness, sores, injuries, peeling or cracking between the toes, pain or a numbness / tingling sensation. Try to wear proper fitting shoes, and any custom made splints, braces and prosthetic devices and to cleanse and moisturize the feet daily.

Lipids and Cholesterol Management
As a diabetic, it is important to modify lifestyle food choices and reduce saturated fat, trans fat and cholesterol intake. Arrangements can be made for you to meet with the care center dietician to improve your understanding of lipid and cholesterol management. Your Primary Care Provider may prescribe medication to assist with lowering high levels of bad cholesterol with drugs called “Statins”. The clinical staff can meet with you to discuss lipid lowering therapy.

STOP Smoking
Medications, counseling, smoking cessation programs and nicotine replacement products (gum, inhaler, patch) increase the chances of stopping. Smoking more than doubles the risk for cardiovascular disease. Smoking tobacco can raise your blood sugar and cholesterol levels as well as raise your blood pressure. Smoking cuts down on the amount of oxygen going through your blood stream to your vital organs and skin. Smoking damages blood vessels, the respiratory tree and lung tissue.
GET HELP. TALK WITH YOUR DOCTOR, FAMILY AND FRIENDS ON WAYS AND STRATEGIES TO STOP.
Consider visiting www.smokefree.gov or call 1-800-QUITNOW (1-800-784-8669). Callers are routed to their state’s quit line or the National Cancer Institute’s quit line.

Eye Care
It is important to report any changes in sight to the clinical staff promptly.
Changes include:
- Blurry or reduced vision
- Symptoms like a curtain rising and falling
- Dark spots
- Flashing lights
- Pain, pressure or light sensitivity
Diabetics have increased risks for serious vision conditions.

Dental Care
Diabetics tend to experience an increase in mouth, gum and tooth problems. Proper mouth care, which includes brushing teeth twice daily can reduce the likelihood of oral complications. During daily mouth care, be observant for the following changes in the mouth:
- White or red oral patches
- Pain, swelling or sensitivity to temperatures or flavors
- Excessively dry mouth
- Swollen, pus or bleeding gums
- Bad breath
- Loose teeth
Regular dental care is important. The dietician can assist you in selecting foods easiest for you to chew and swallow.

Heart and Circulation Health
Management of blood pressure has proven to reduce diabetic complications. More than 75% of diabetics have some form of heart or circulatory disease. Controlling high blood pressure in the diabetic is essential in reducing heart disease, strokes, kidney and eye disease risks. Your Primary Care Provider may prescribe medications that will alter blood pressure, urination and control blood clotting times. The clinical staff will monitor your vital signs and blood tests during your stay at the care center.

Depression Management
Diabetics, especially those suffering diabetic complications have increased risk of developing clinical depression. Please talk to our staff if you experience the following feelings:
- Sleeping too much or not enough
- Eating too much or not enough
- Increased aches and pains
- Lack of energy or motivation
- Increased irritability, restlessness and intolerance
- Loss of interest in things of pleasure
- Isolation
- Feeling worthless and joyless
- Poor concentration
- Thoughts of death or suicide
Rehabilitation includes both physical and mental health. The care center can make arrangements for you to receive professional mental health counseling, if deemed necessary by your Primary Care Provider. Staff may provide medications to assist with behavior and mood changes, monitor medication blood levels and assure support from social workers and clergy, if desired. It is essential to take time and enjoy life. Professional mental health services may improve your mood and energy level.
If you found an error, highlight it and press Shift + Enter or click here to inform us.